Testing menstrual blood collected on a standard sanitary pad can detect high-risk human papillomavirus (HPV) with accuracy comparable to clinician-collected cervical samples, supporting its potential use as a non-invasive alternative for cervical cancer screening.
The finding comes from a large community-based study in China that evaluated whether HPV testing from menstrual blood could reliably identify high-grade cervical disease. The study, published in BMJ, suggests that a routinely discarded biological sample may be suitable for primary HPV screening without compromising diagnostic performance.
HPV testing is already the cornerstone of cervical cancer prevention, but uptake remains uneven, particularly in low-resource or underserved settings. Barriers include limited access to trained clinicians, discomfort with pelvic examinations, and sociocultural concerns around invasive sampling. Self-sampling approaches such as vaginal swabs have improved participation but still require active specimen collection and handling. Menstrual blood testing offers a different model, aligning sample collection with normal physiology rather than a clinical procedure.
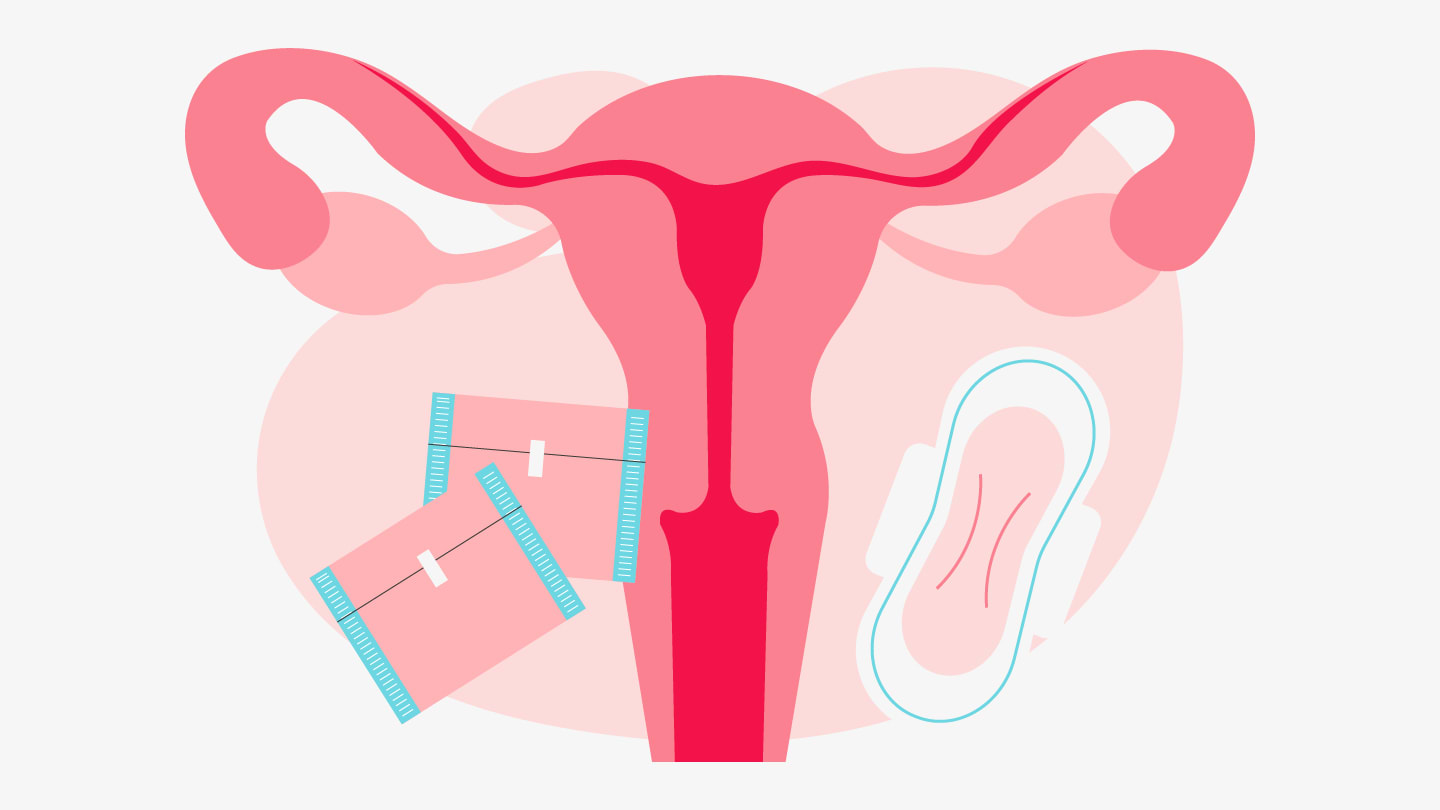
In the study, more than 3,000 menstruating women provided both clinician-collected cervical samples and menstrual blood samples collected using a small standardized strip attached to a sanitary pad. HPV genotype testing on menstrual blood demonstrated similar ability to rule out clinically significant disease as clinician sampling, with very high negative predictive value for high-grade cervical lesions. From a screening perspective, this means a negative menstrual blood HPV test could offer strong reassurance that serious disease is unlikely.
Although menstrual blood testing showed slightly lower specificity than clinician sampling, referral rates for follow-up procedures were comparable between methods. This balance is critical for laboratories and screening programs, as excessive false positives can strain colposcopy services, while missed disease undermines screening goals. The study’s results suggest menstrual blood testing could be integrated into existing diagnostic pathways without substantially increasing downstream workload.
Menstrual blood samples were compatible with existing HPV DNA testing platforms, and processed using defined protocols. Importantly, the approach does not require new molecular targets or complex assay redesign, focusing instead on an alternative specimen type.
If adopted more widely, menstrual blood HPV testing could expand screening coverage by enabling home-based collection without vaginal instrumentation, particularly in populations with limited access to clinical care. In diagnostics, this work highlights an opportunity to support cervical cancer prevention through flexible sampling strategies that maintain analytical performance while lowering barriers to participation.




